Events
Check out our calendar of events and participate in our seminars, public lectures, and information sessions.
Dr Samantha Barton - The Florey Institute »
Dr Samantha Barton will present 'Using iPSC-derived Organoids to Model MND and MS'.
Dr Kirsten Fairfax - The University of Tasmania »
Dr Kirsten Fairfax will present 'Immunogenetics'.
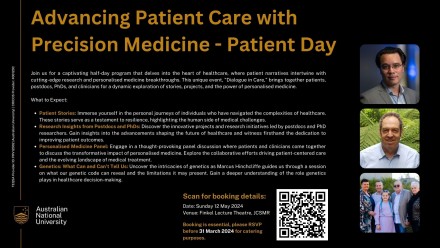
Pathways to Precision: Empowering Patient Care through Genomics - Day One »
Uncover the transformative power of functional genomics and phenomics at our exclusive workshop. Explore how clinicians leverage cutting-edge research to revolutionise patient diagnoses and treatments.
Pathways to Precision: Empowering Patient Care through Genomics - Day Two »
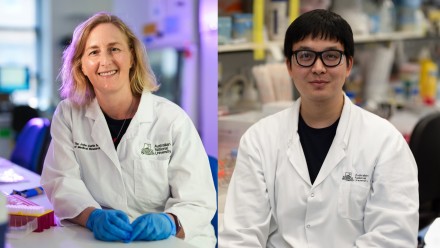
Join us for a captivating half-day program that delves into the heart of healthcare, where patient narratives intertwine with cutting-edge research and personalised medicine breakthroughs. This unique event, "Dialogue in Care," brings together patients, postdocs, PhDs, and clinicians for a dynamic exploration of storie
Professor Leonie Quinn - The John Curtin School of Medical Research (ANU) »
Professor Leonie Quinn will present 'Solving mysteries of the neural stem cell niche to understand brain cancer'.
Professor Maher Gandhi - Executive Director, Clinical Research at Mater Research Institute »
Professor Maher Gandhi will present 'The lymphoma microenviroment and its many manifestations.'
CHOIR Speaker Series - Panel Discussion »
Topic: Consumer engagement in clinical trials.
Associate Professor Naomi Hammond - Program Head, Critical Care Division, The George Institute »
Associate Professor Naomi Hammond will present 'Clinical trials in critical care – the road to success.'